Patients often ask if sports tape can be used to treat a condition, in place of customised foot orthotics. Sometimes this arises out of financial considerations, and other times because they do not understand the specific roll that a taping procedure plays when treating lower limb biomechanical dysfunction.
Practitioners can incorporate taping therapy into their treatment regimes to help patients who may be unsure of the value of orthotic therapy, and so identify whether orthotic therapy will be of benefit. Sports taping techniques can be incorporated in conjunction with orthotic therapy for a period of time to provide optimum results for the patient.
There are numerous conditions for which a taping procedure can be beneficial such as, Plantar Fasciitis, Osgood Schlatter condition and knee pain (Chrondromalacia Patella syndrome).
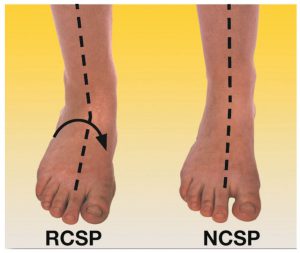
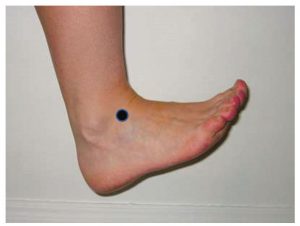
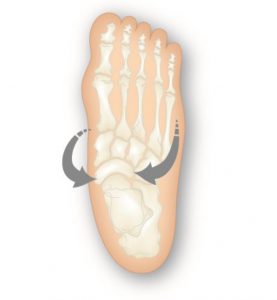
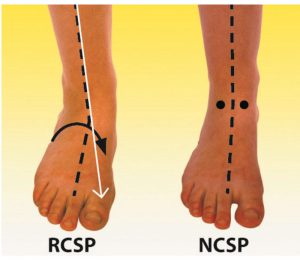
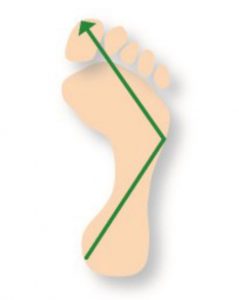
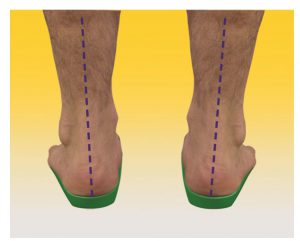
Plantar Fasciitis ( heel spur syndrome) is a classic case where the use of a low dye strapping technique is particularly effective as a temporary treatment to ‘mimic’ the realignment and support provided by an orthotic device. ‘Low dye’ taping seeks to control the foot and lift the longitudinal arch at the susentacula tali area, to limit excessive calcaneal eversion. The mechanism used controls the rearfoot, lifts the arch, shortens the foot structure, which in turn reduces the elongation of the plantar fascia and tension at the calcaneal attachment.
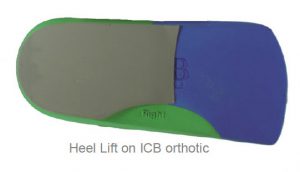
This method of treatment is very effective, however, the sport tape must be replaced within 3-4 days, some patients have allergic reactions to the zinc oxide tape. Low dye taping is especially effective for long term foot pain sufferers, such as Severs Disease and patients with Achilles Pain, when used in conjunction with an orthotic device.

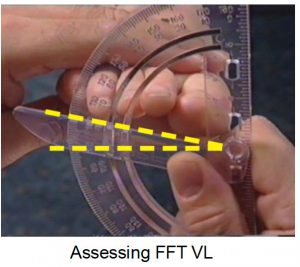
Note in figure 1 (below) how the tape is crossed over in a ‘figure of eight’. Watch the video below for the Low Dye Strapping technique.
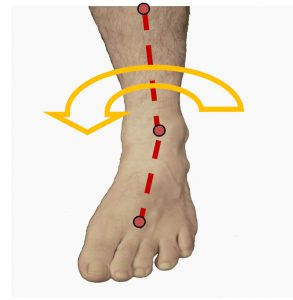
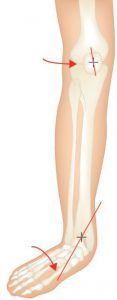
Osgood Schlatter Condition is one which responds very quickly to a combination of orthotics (to treat the excessive pronation) and strapping (to reduce tension on the patella tendon). The complicating issue with Osgood Schlatter is external tibial torsion, which should be treated by a practitioner who uses ‘gait plate’ orthotic therapy to correct the torsion. Growth spurts combined with excess pronation, a highly active child and external tibial torsion are all contributing factors.
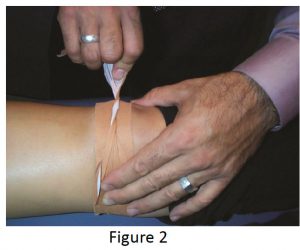
Strapping may be used exclusively to treat to Osgood Schlatter (see fig. 2 ). However the condition and associated pain often appears to ‘flare up’ and so controlling the patients’ biomechanics is essential for effective treatment.
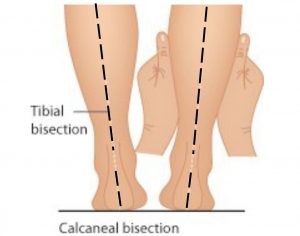
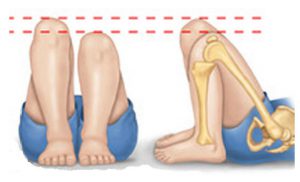
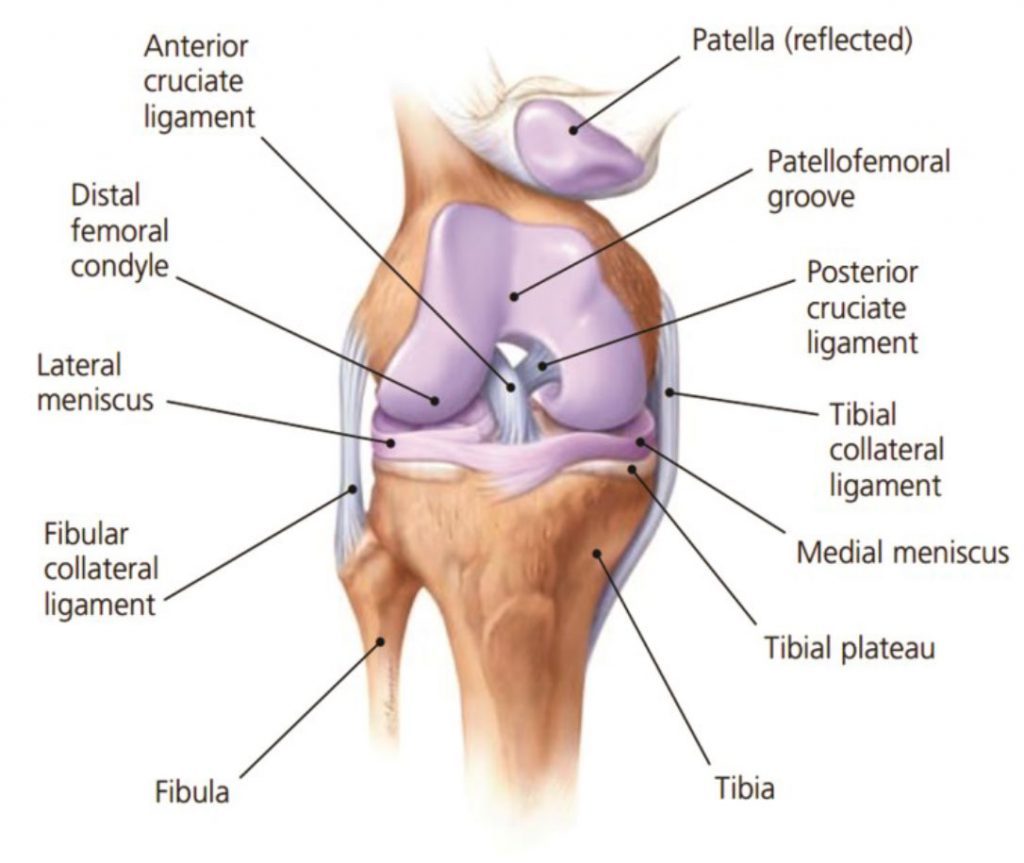
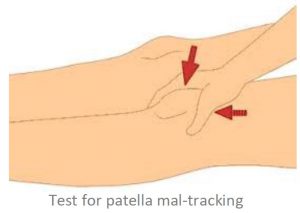
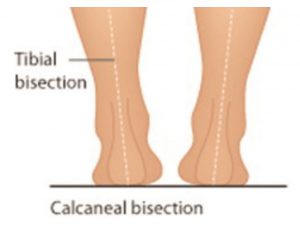
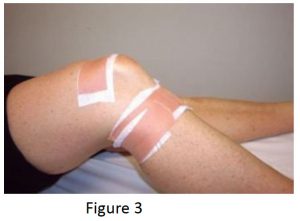
Medial knee pain due to excessive pronation can be assisted using orthotic therapy and the McConnell strapping techniques to stabilise the patella. Internal tibial rotation is associated with excessive pronation, resulting in medial displacement of the patello-femoral path and encouraging lateral displacement of the patella (knee cap). See Fig 3 below This is a common problem and elicits pain and around the medial aspect of the patella, especially with excess loading activities such as running.
Internal tibial rotation is also responsible for creating medial collateral strain of the ligamentous structures that wrap around the medial aspect of the knee and lower leg (Cosgarea, 2002).
Excessive pronation causes excessive strain to the medial co-lateral ligament. As a factor of this condition the VMOs weaken and the ITBs tighten, causing external rotation of the femur as a compensation. The patella begins to track on the lateral aspect of the femoral condyle, crepitation and grating feeling is experienced on flexion to extension.
As mentioned strapping using the McConnell technique and strengthening the VMOs is a good treatment regime, however, it will NOT correct the cause of the problem, only assist in pain relief.
Anecdotal studies have supported that in clinical practice, patellar tape provides a useful treatment technique, clinical and research evidence supports relief of pain associated with PFPS (patella femoral pain syndrome)1 The condition and pain will generally recur constantly until the knee has degenerated or become OA (osteoarthritic) – at which time surgical intervention may be needed.
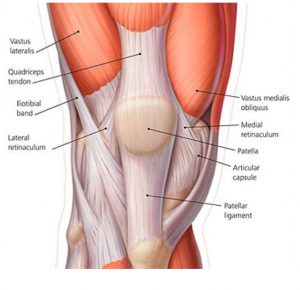
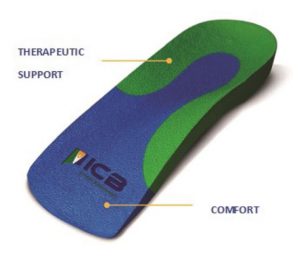
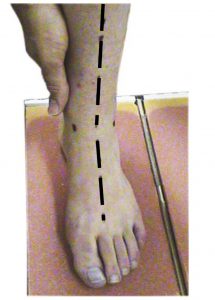
A basic requirement to reduce rotational stress on the knee is control and correction of the STJ (Subtalar Joint) and MTJ (Midtarsal Joint) pronation and this can be achieved with an orthotic device that corrects rearfoot pronation.
The most effective biomechanical treatment for medial knee pain, involves the following 3 steps:
1. McConnell Technique – to control lateral/medial patella displacement.
2. Low Dye Strapping – to mimic orthotic treatment. However, low dye is only a temporary treatment.
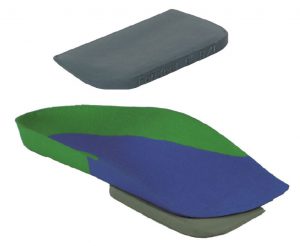
3. Orthotics to stabilise the structure and limit excess pronation. The orthotics should be moulded to the patient’s NCSP (Neutral Calcaneal Stance Position) Otherwise described as Ideal position.
This action will control STJ and MTJ pronation – making it more effective in producing long term results for the patient.

REFERENCES :
1. Patellar taping: is clinical success supported by scientific evidence K. Crossley*, S. M. Cowan*, K. L. Bennell*, J. McConnell. Manual Therapy (2000) 5(3), 142-150
COSGAREA, A.J., BROWNE, J.A., KIM, T.K. & MCFARLANE, E.G. (2002) Evaluation and Management of the Unstable Pa-tella, The Physician and Sports Medicine, 30, 10