One issue that often surfaces when using orthotic products is, whether there is a need to heat mould and apply additions or grind and modify the orthotics?
SAVE 10% OFF ICB PRODUCTS WITH DISCOUNT CODE: 02ICB10 Offer online only!
The question of heat moulding often arises and the answer is simply, it may not be necessary in every situation. However, heat moulding does assist in avoiding patient compliance issues.
Using additions to improve the treatment of the basic orthotic foot bed, is one, in which many practitioners are not that familiar with in the modification process.
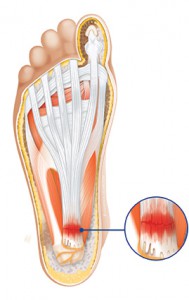
Most additions are used to treat specific conditions by providing the support which has been lost, such as: metatarsal domes to support the transverse arch or a heel lift to support a short leg.
Many orthotic manufacturers promote their products as being one which can be taken from the display pack and placed in the shoe with no further alteration needed. This may be so for some patients, however, simple adjustments may provide the necessary comfort and treatment result the patient requires.
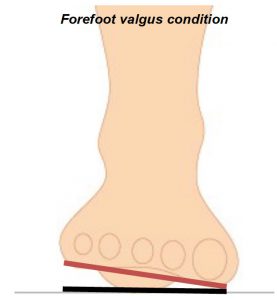
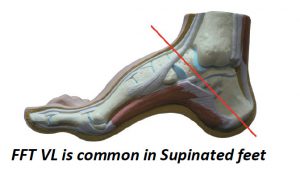
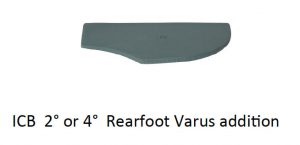
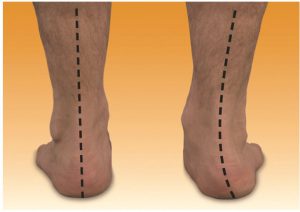
A key element to achieving a satisfactory treatment commences with checking that the ‘off the shelf’ orthotic contains at least a basic rearfoot varus angle to enable correct alignment for the patient.
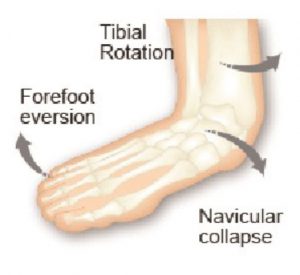
Products available in pharmacies often only provide arch support without attending to rearfoot (calcaneal) control.
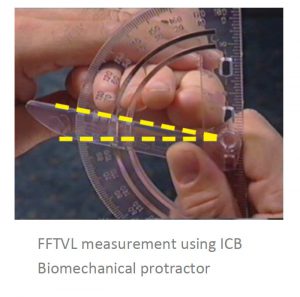
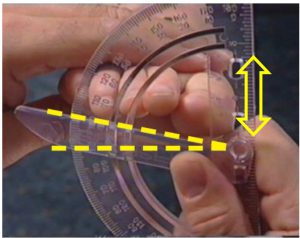
Practitioners should check the rearfoot position by simply viewing and where necessary measuring, using a biomechanical protractor.
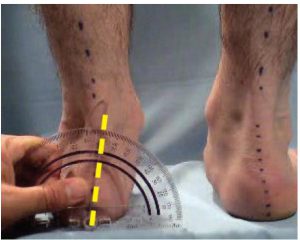
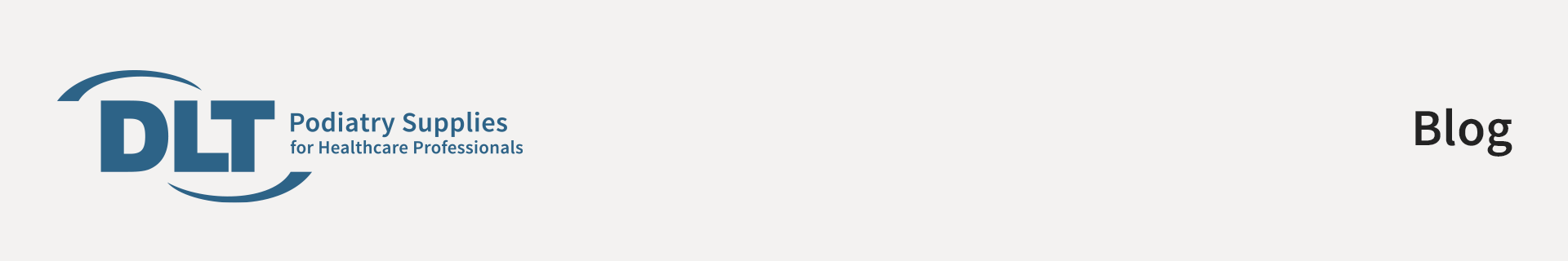
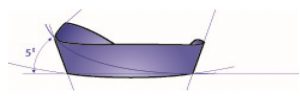
ICB heat mouldable orthotics exhibit a 50 rearfoot varus post to align the calcaneus with the average tibial varum angle, thus placing the foot into the patients ideal position.
Reducing excess pronation can have substantial benefits, such as reducing internal tibial rotation.
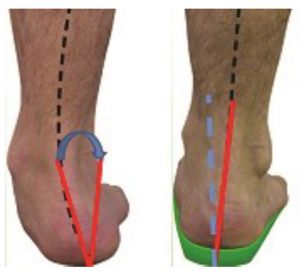
The product that a practitioner chooses to use, should be one which is easy to modify and alter, thus providing the necessary treatment requirements. For example, ability to incorporate an intrinsic dome into the orthotic device, thus providing the patient with a product with increased functionality or provide more comfort to the wearer.
Use a heat gun to mould the dome into the plantar surface. (see other videos on Youtube)
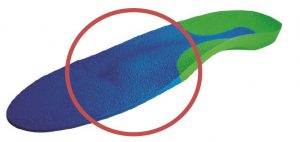
Simple add on additions, such as, medial flanges can reduce medial rubbing of the foot on the shoe or provide increased support for patients such as CP suffers and excessive pronators can be quite useful.
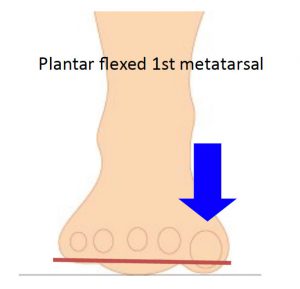
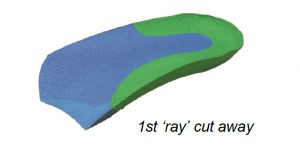
For practitioners who want to modify the actual orthotic by grinding , there are many simple adjustments that can be made, such as a deflection for a plantarflexed 1st . (see below)
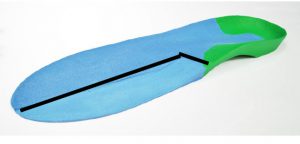
Pictured below is a 1st metatarsal deflection for a 2/3 or 3/4 length orthotic.
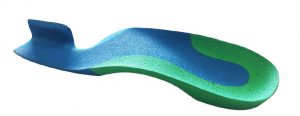
The ability to adjust and modify the product within the clinic can be a great asset. The product should have the ability to be modified by either application of heat (using a heat gun) and also be a material that can be ground and shaped using either bench grinders or hand grinders.
(above) Deflection for dropped metatarsal heads using heat and a spoon to create a depression .
For those practitioners with higher hand skills the grinding option is fast and extremely effective.
One very useful modification is the use of a full length ICB orthotic product to fashion a Morton’s ramp in which toe separator is an incorporated feature.
The steps to creating this modification are as follows:
Step 1
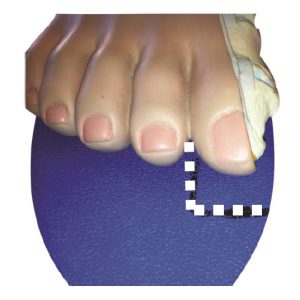
Mark the distal position of the ramp, 5mm distal to the hallux.

Step 2
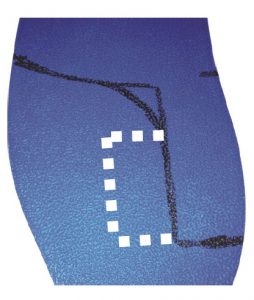
Mark out the Morton’s ramp ensuring that it sits between the hallux and the 2nd phalange.
Step 3
Add the toe separator shape and cut to shape.
Step 4
Use the heat gun and the grinder to position the toe separator and smooth down the edges.