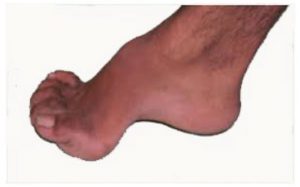
The term Pes cavus is derived from Latin meaning ‘hollow foot’ and covers a wide spectrum of foot deformities.
The Pes cavus foot can be hereditary or acquired and the underlying causes can be neurological, orthopaedic or neuromuscular. The condition can be wide ranging from conditions such as Chartcot-marie-tooth disease (CMT) and Fiedreich’s ataxia to the more commonly high arched supinated foot acquired from familial predisposition.

The CMT foot symptoms are progressive and can include :
• Ankle weakness
• High arches
• Clawed toes
• Muscle wasting
• Poor balance
• Muscle weakness in hands and feet
• Peripheral neuropathy

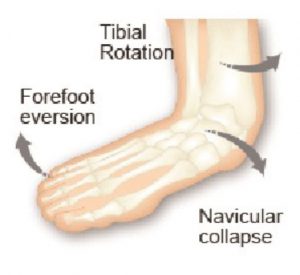
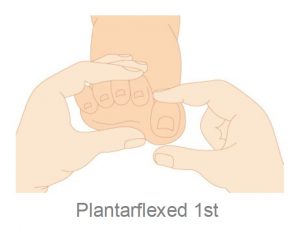
More commonly the condition is not so severe and is generally characterised by an abnormally high medial longitudinal arch, is described as a high axis foot and is most commonly associated with a high forefoot valgus deformity. Other features often include a varus (inverted) calcaneus, a plantarflexed position of the first metatarsal and adducted forefoot together with dorsal contracture of the toes or hammer toes.
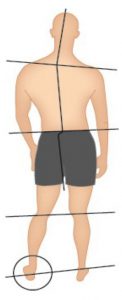
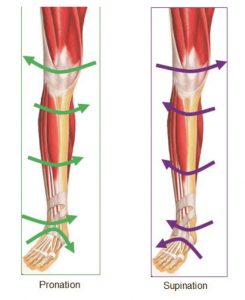
Pes cavus feet will invariably be identified as supinated feet and characterised as having ‘reduced or limited pronation’.1 Population-based studies suggest that the prevalence of the cavus foot is approximately 10% 2 .The high arched cavus foot has a decreased range of motion, increased stiffness, and decreased pronatory compensation1.
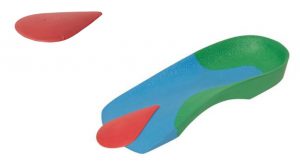
Often this type of foot will exhibit increased rearfoot varus together with a higher incidence of lateral instability of the foot and ankle1.
Valmassy3 outlines 6 characteristics of a cavus foot:
1) Limited pronation
2) Rigidity
3) Uneven weight distribution
4) Digital contractures (clawing of the toes)
5) Increased tendency to lateral ankle instability with associated ankle sprains
6) Decreased ankle joint dorsiflexion(osseous block)

Inversion Sprain
Valmassy3 states that besides the genetic predisposition or familial predisposition other causes to this condition are many and varied such as: Congenital plantarflexed 1st Ray deformity; spasm of peroneus longus; spasm of posterior tibial; weakness of peroneus brevis; weakness of peroneus longus; clubfoot deformity; metatarsus adductus. Underlying causative factors may include but not limited to: Charcot-Marie-Tooth disease, Friedreich’s ataxia, poliomyelitis, spina bifida to name a few.
A study of painful Pes Cavus feet ‘indicates that custom foot orthoses are more effective than a control for reducing cavus foot pain and associated limitation in function.
The key feature of a successful orthotic device for this patient population is a contoured flexible shell moulded to the exact morphology of the foot, with a full-length cushioned top cover. Such a device has the effect of reducing and redistributing abnormal plantar pressure loading. For patients presenting to the clinician with painful cavus feet, custom foot orthoses are an effective treatment option 2.

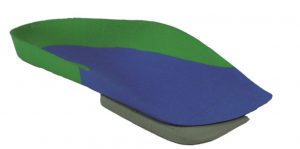
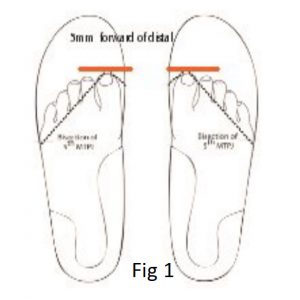
Commonly Pes cavus feet present with Forefoot Valgus deformity (FFTVL) and it is wise in the assessment to complete a FFTVL assessment.
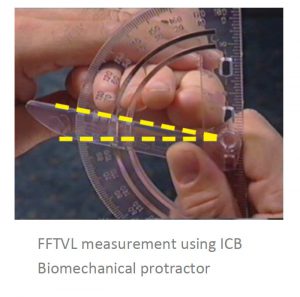
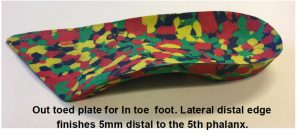
Use a forefoot valgus addition on the orthotic to reduce forefoot instability and lateral inversion of the foot by locking the 4th and 5th columns to mimic ground reaction forces.
High arched feet do not usually require a rigid orthotic support, rather a softer accommodative device such as soft or mid density EVA materials.
However, it is important to mould the orthotic well into the arch and use a metatarsal dome to reposition and lift the transverse arch if the toes are clawing.