Sesamoiditis is painful inflammation of the sesamoid apparatus, which is located in the forefoot under the 1st MTPJ. It is not a particularly common condition and can be at times difficult to diagnose and treat. Generally it is accepted that the sesamoids perform two principal functions:
1. Absorbing impact forces in the fore-foot during walking through a series of attachments to other structures in the forefoot.
2. Acting as a fulcrum to provide the flexor tendons with a mechanical advantage as they pull the hallux down against the ground during gait.
Watch the short video below
The hallux (big toe) has two phalanges and two joints (interphalangeal joints), together with two small sesamoid bones (the medial and lateral sesamoid bones).
The sesamoids are implanted or embedded in the flexor hallucis brevis tendon which exerts pressure from the big toe against the ground and aids in the act of walking during the toe-off phase of gait. The sesamoids not only have to endure the pressure of body, weight and gravity, but also the constrictive pressure of the flexor hallucis brevis tendon.
There are generally five categories of sesamoid apparatus type injuries:
A. Sesamoiditis is a general description of the condition which is given to inflammation of the sesamoids but actually relates more specifically to tendonitis of the flexor halluces longus1.
B. Stress fractures of the sesamoid usually occurring as an impact injury.
C. Acute sesamoid fracture most commonly an evulsion fracture.
D. Osteochondritic dissecans or avascular necrosis. A feature in which the blood supply to the sesamoid bone is interrupted in which bone death can result.
E. Chondromalacia of the sesamoid resulting from continual synovitis of the 1st MTPJ in which fibrosis develops leading to freezing of the sesamoids1 and apparatus.
Sesamoiditis is the most common and is characterised by pain at the first metatarsal sesamoid commonly occurring in combination with a plantar flexed 1st metatarsal. This condition may present as often as in 4% of overuse type foot injuries (Dennis and McKinney, 1990).
Sesamoiditis typically affects physically active young people and is more common in sporting people who require to balance on the ball of the foot (such as ballet dancers, basket ballers, netballers, cricket players and soccer players) – as they attempt to stop and change direction by pivoting or putting pressure on the forefoot area and the 1st MTPJ.

The condition causes pain under the 1st MTPJ and commonly affects the medial (inner) side of the joint. The pain may be constant, or it may occur with or be aggravated by, movement of the big toe joint. It may also be accompanied by swelling (oedema) throughout the plantar aspect (bottom) of the forefoot.
It is reputed that the forefoot bears approximately one half the body’s weight and balances pressure on the ball of the foot. Sesamoiditis has been also linked as a possible uncommon cause to Metatarsalgia2.
It is generally accepted that the sesamoids perform two principal functions:
1. Absorbing impact forces in the forefoot during walking through a series of attachments to other structures in the forefoot.
2. Acting as a fulcrum to provide the flexor tendons with a mechanical advantage as they pull the hallux down against the ground during gait.
Patients who suffer from Sesamoiditis often exhibit a fixed or mobile plantar flexed 1st metatarsal which maintains the 1st MTPJ on impact. The lesser metatarsals absorb the impact in the gait cycle, however, if the 1st MTPJ is rigid and the sesamoid take the full impact during toe off. Repetitive chronic pressure and tension on the forefoot will cause the surrounding tissues to become irritated and inflamed. In some cases the sesamoids may bifurcate and in severe cases necrosis may occur.
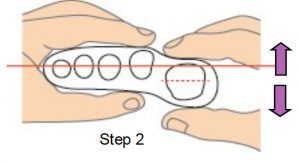
The practitioners should check the patient for a Plantar flexed 1st using the common test in which the movement of the joint should be 5mm dorsiflexion, and 5mm plantar flexion or a total range of approx 10mm.
This test will identify if there is a limitation in the joint’s range of motion due to a fixed osseous condition.
How to perform this test:
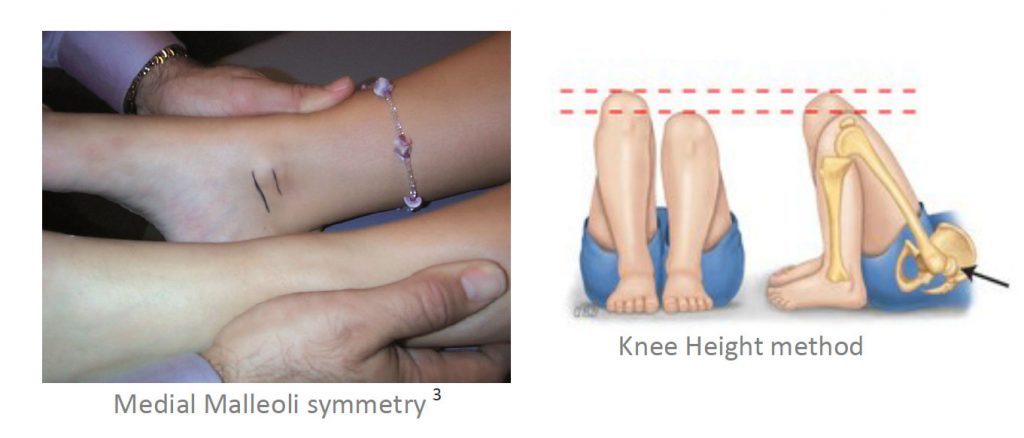
1.With the patient in the supine position, maintain the foot in the neutral position, using ICB Anterior Alignment Method.
2. Grip the lesser metatarsals, line the thumbs up and the range of movement should be 5mm up and 5mm down.
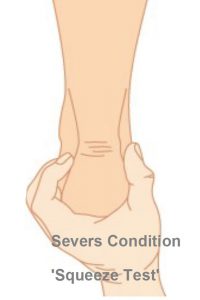
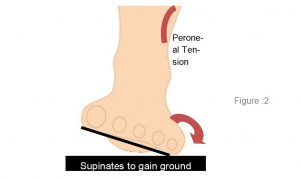
Pronation will displace the sesamoids laterally causing trauma to the sesamoid apparatus. This can change the patient’s gait as they try to compensate and may cause other upper body compensatory effects, including hip pain.
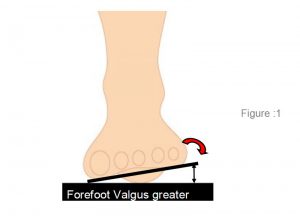
A Supinated foot will often display a plantar flexed 1st as compensation to assist in lowering the 1st MTPJ to the ground and thereby enabling toe off.
Patients who suffer from Sesamoiditis may exhibit a fixed or mobile plantar flexed 1st metatarsal 3 which maintains the 1st MTPJ in a plantar flexed position on impact. The lesser metatarsals are able to absorb the impact in the gait cycle, however, the 1st MTPJ is rigid and the sesamoid take the full impact during toe off.
Repetitive chronic pressure and tension on the forefoot will cause the surrounding tissues to become irritated and inflamed. In some cases the sesamoids may bifurcate and in severe cases necrosis may occur.
Treatment
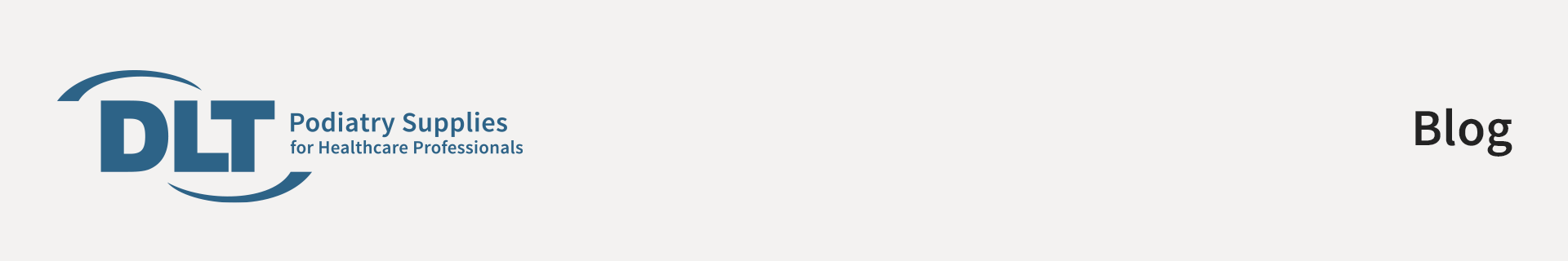
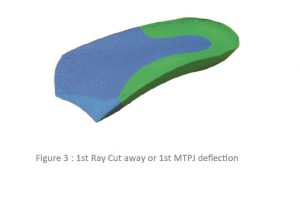
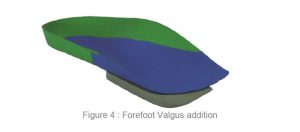
Initial treatment for sesamoiditis is usually non-invasive and includes orthotic therapy to treat the plantar flexed 1st. Generally a deflection will need to be incorporated into the orthotic to remove or reduce the pressure from this area.
The Plantar flexed 1st Ray (metatarsal) deflection is cut around the 1st MTPJ and then the edges are heated and smoothed to taper the edge of the orthotic, and avoid irritation (see opposite). The orthotic itself has some in-built forefoot support under the 2nd to 5th to support this area similar to a 2-5 bar.
Treatment is generally non-surgical, however, if conservative measures fail, surgical intervention by way of removal or pinning of the sesamoids may be undertaken.
Modifying the patients’ shoes is not overly effective as each pair would need to be modified. The easier approach a heat mouldable orthotic incorporating a Plantar flexed 1st ray deflection modification which can be moved and transferred from shoe to shoe with relative ease.
In addition, the big toe may be bound with strapping tape (or athletic strapping) to immobilise the joint as much as possible and allow healing to take place.
Acupuncture can be used to reduce inflammation and anti inflammatory drugs can be taken to reduce swelling.
If a full length orthotic is required a ‘relief trench’ can be placed into the orthotic using a dremel hand grinder to allow the 1st MTPJ to plantar flex without restriction.
Differential Diagnosis:
• Stress fracture of the sesamoid bone
• Avulsion fracture or sprain of the proximal pole of the sesamoid
• Sprain of the distal pole
• Sprain of a bipartite sesamoid
• Arthrosis of the sesamoid metatarsal articulation. Arthrosis pain is often felt during the day and emphasises during joint movement efforts
• Pre-radiographic osteonecrosis of the sesamoids