Posterior tibial tendon dysfunction (PTTD) is a condition that results in inflammation or tearing of the posterior tibial tendon.
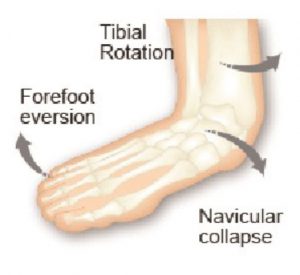
The Tibialis Posterior is an inverter and plantar flexor of the foot1. The Posterior Tibial Tendon is the major dynamic stabiliser of the foot in pre-venting rearfoot eversion or pronation and is subject to repetitive overuse injury such as, peritendinitis, inflammation of the tendon sheath, and rupture2. Often the early stages of the condition can be overlooked or misdiagnosed3.
PTTD can be experienced bilaterally and or unilaterally, typically beginning with a paratenonitis of the tendon which may lead to synovitis, intrasubstance tearing and tendinosis4. ‘Recent literature has reported a higher prevalence of PTTD in women than in men, but with no explanation for this discrepancy’5.
It is suggested that there are numerous underlying causative factors such as: excessive pronation, trauma, anatomical anomalies (eg. leg length discrepancy), inflammatory joint diseases, acute evulsion, iatrogenic events to name a few.
Many commentators state that PTTD is an overuse condition as the symptoms usually occur after activities that involve stress on the tendon, such as running, walking, hiking or climbing stairs.
The condition has often been categorised as ‘adult acquired flatfoot’ and research concludes that PTTD results in loss of medial arch structure and abduction of the forefoot, resulting in a change of gait4, accompanied by ensuing upper structure issues.
PTTD is categorised as having 3 stages of progression, the duration and severity can move rapidly from acute phase to subacute phase and ultimately chronic. The symptoms of PTTD can include pain and swelling. As PTTD advances, eversion of the calcaneus occurs and the arch often flattens, shifting pain to the lateral aspect of the foot (below the ankle). As the tendon deteriorates arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
A recent study of PTTD Phase 2 patients suggest that non-surgical treatments to consider include reducing Posterior Tendon activity using arch supports/foot orthotics4 and inverting the rearfoot using an orthotic device with an Increased rearfoot varus angle. Inverting the entire orthotic device using an ‘inversion ramp’ can significantly reduce strain on the tibialis tendon.
ICB Full Length orthotic fitted with inversion ramp.
The ICB ramps are available in 4°,6°,8° and are 32cm in length.
Conservative Treatments
• Immobilisation: short-leg cast or ‘moon boot’ to allow the tendon to recover.
• Ultrasound therapy and exercises may help rehabilitate the tendon and reduce inflammation.
• Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) to reduce the pain and inflammation.
• Foot Orthotic Devices: to reduce calcaneal eversion/pronation are effective in stages 1-3. The addition of a medial flange to the dorsal arch of the orthotic can provide extra support to the navicular.
• Footwear: Shoes that are designed with a flat base that provide good mid foot control and heel cup support can reduce arch collapse. In cases of PTTD that have progressed substantially or have failed to improve with non-surgical intervention, surgery may be required.
References:
1. Merriman’s Assessment of the Lower Limb (2008), 3rd Edition. Churchill Livingstone. p264 2. Plattner PF (1989) Tendon problems of the foot and ankle. Postgraduate Medicine 86(3):155-170 3. Wassef S., Mikhail M., (2008) Ankle, tibilais posterior tendon injuries. Available at: http:// emedi-cine.medscape.com/article/ 386322-overview 4. S.I. Ringleb, S.J. Kavros, B.R. Kotajarvi, D.K. Han-sen, H.B. Kitaoka, K.R. Kaufman Changes in gait associated with acute stage II posterior tibial tendon dys-function Gait & Posture 25 (2007) 555–564 Biomechanics Laboratory, Division of Orthopedic Research, Mayo Clinic College of Medicine. 5. Gehrig Laura MD, Posterior Tibial Tendon Dysfunction: More Prevalent in Women, AAOS Now, Issue: March 2009