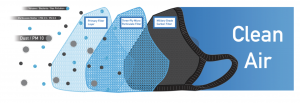
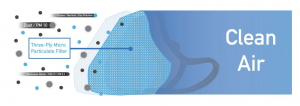
Cambridge Masks filter air through three different layers . . .
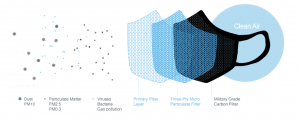
The first layer of the Cambridge Mask filters out larger particles such as dust and PM10. The material is sublimation printed in different patterns to make the masks fashion friendly.

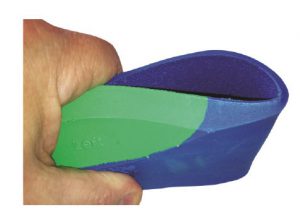
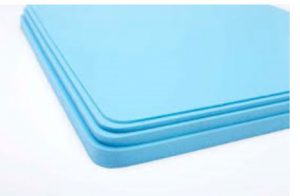
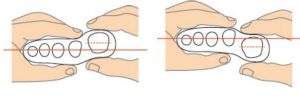
The second layer of the mask blocks particulates such as PM2.5. It also filters 99.79%+ of particles as small as PM0.3. The textile is a three-ply non-woven melt-blow polypropylene, a thermoplastic polymer used in a range of applications.
The blow moulding process begins with melting down the polymer and forming it into a “parison” – a ball of liquid. High velocity air is then passed through to attenuate the filaments and create a fibrous web. The random fibre orientation this triggers is advantageous because it creates a better mesh to trap particles. The textile is also created with a high surface area, meaning a greater percentage of particulates are captured as they pass through the filter.
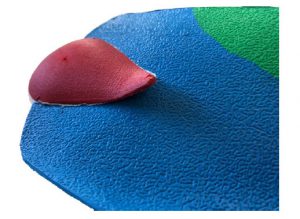
The Cambridge Mask Pro is completed with the inner filter which is made from a 100% pure activated carbon cloth, which was originally invented by the UK Ministry of Defence. It was then extensively developed and made into a product for use in chemical, biological and nuclear warfare protection, of the type used by armed forces around the world. We hold the exclusive global rights for this material for use in a consumer pollution mask. You won’t find it in any other mask outside of the military.
All activated carbons – traditionally powders and granules – generate “Van der Waal” forces due to their porous structure. These forces give activated carbons their unique potential to adsorb gaseous molecules, including anions and cations into their internal pores.
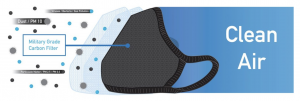
Our filter material is comprised of a series of activated carbon filaments, each about 2,000 nanometres in diameter. Each filament is many times smaller than the typical grain size in standard carbon materials, making the rate of adsorption of pollutant gas much faster and therefore more powerful. It also means that bacteria and viruses are drawn to the filament surface much more efficiently, because there is so much more available surface than in a granular carbon.
The high number of filaments – spun into a yarn and then woven into cloth – makes the speed of adsorption extremely fast in a material that is still easy to breathe through. Not only are molecules such as pollutant gases and endotoxins quickly adsorbed into the pores from a much wider area, but the Van der Waals forces also attract and immobilise on the filament surface much larger particles including bacteria, which often have a negatively charged membrane. Together with the anti-bacterial silver added to the filament surface, the activated carbon cloth traps the bacteria and draws out the gel-like cytoplasm inside – killing it and preventing infection.
Cambridge Masks are therefore powerful respirators that not only clear the air of pollution via the particulate filter, but also remove potentially harmful gases and pathogens with the additional carbon filter.