The question is of course: What is regarded as success?
When dealing with Orthotic therapy we are not attempting to heal and often we are not attempting to eradicate the biomechanical issue. Rather we are working within the parameters of a mechanical device to provide the patient with short, mid and long term relief to the pain and discomfort that they are suffering. We also may offer a method to stop an issue progressing to the next level.
Orthotic therapy is NOT a ‘cure all’ for every disease, however, when used in combination with other treatment modalities, can provide improved gait, reduce pain, assist in providing an enhanced quality of life to patients.
There is a wealth of information attesting to the benefits of orthotic therapy for a wide range of biomechanical conditions, such as:
• Hallux Abducto Valgus (bunions): commonly caused by a short 1st metatarsal shaft and aggravated by excessive pronation.

• Ball of Foot Pain: collapsing and rotating of the metatarsals caused by pronation.
• Plantar Fasciitis & Heel Spur: excess pronation causes the fascia to elongate and tear at the attachment to the calcaneus. An inferior calcaneal spur is a secondary compensation, in which an osseous growth develops at the attachment to secure the fascia.
• Achilles Pain: repetitive over-stretching of the medial and lateral attachments of the Achilles tendon caused by both pronation and or supination, create a point of pain or stress point.
• Severs Disease (children’s heel pain): related to pronation and growth spurts in children and affects active sporting children more than sedentary ones
• Shin Splints (lateral, medial or an-terior): pronation and supination can be key contributing factors.
• Knee Pain: and collateral ligament strain due to pronatory and supinatory factors and or forefoot anomalies.
• Osgood Schlatters Syndrome (children’s knee pain): occurs due to a combination of tibial torsion, growth spurts and pronation factors.
Hip Pain: due to structural or functional leg length difference and supination/pronation factors including tight external hip rotators and structural long leg compression into the acetabulum.
Low Back Pain: unilateral and bi-lateral pronation and structural and functional leg length difference causing stress on the lower back L1-L5.
Leg Length Syndrome: when a structural leg length difference is evident the long leg may excessively pronate to level the pelvis.
A report by The American College of Foot & Ankle Orthopaedics & Medicine titled ‘Prescription Custom Foot Orthoses – Practice Guidelines’,1
Gives a wider and more comprehensive array of conditions when in their opinion are able to benefit from the application of prescription orthotic products. The ICB heat mouldable range of orthotics are a simple, cost effective efficient way to treat your patients with customised prescription orthotics and do it right in your own private clinic.
The quoted report lists
1. Proximal Lower Extremity Pathology: A. Shin Splints, B. Tendonitis (Tenosynovitis), C. Posterior Tibial Dysfunction, D. Chondromalacia Patella (Runner’s Knee, Patellofemoral Syndrome), E. Iliotibial Band Syndrome, F. Limb Length Discrepancy
2. Arthritides: A. Inflammatory Arthritis, B. Rheuma-toid Arthritis, Psoriatic, C. Arthritis, Other Inflammatory Arthritides, D. Osteoarthritis.
3. Mechanically Induced Pain and Deformities: A. Pes Cavus, Haglund’s Deformity , B. Hammer Digit Syndrome, C. Functional Hallux Limitus, Hallux Limitus and Hallux Rigidus, D. Plantar Fasciitis, E. Equinus, F. Sinus Tarsi Syndrome, G. Tailor’s Bunion (Bunionette), H. Hallux Abducto-Valgus (Hallux Valgus, Bunion), I. Pes Planus, J. Metatarsalgia, K. Sesamoiditis, L. Morton’s Neuroma (Intermetatarsal Neuroma).
4. Paediatric Conditions: A. Calcaneal Apophysitis, B. Genu Varum and Genu Valgum, C. Tarsal Coalition, D. Metatarsus Adductus.
The issue of success is really not in question, rather when where and how to use orthotics to benefit the patient is!
There are then 3 main questions regarding orthotic therapy to ask when treating patients and these are :
1. Does the patient present with a condition that has been reported to be successfully treated with orthotics?
2. Does the patient present with asymptomatic lower limb biomechanical anomalies or faulty foot mechanics? The patient can also be presented with orthotics as a preventative or prophylactic treatment.
3. Will the support and stabilisation offered by orthotic therapy enhance the overall treatment outcome? This is a personal, clinical determination to be made by the practitioner.
A consideration is:
The cost of prefabricated heat mouldable foot orthoses is relatively low, and the adverse effects of using foot orthoses are minor. (see below 2,3).
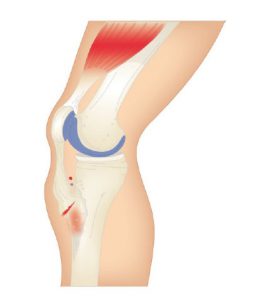
There are 3 key starter steps in orthotic therapy:
SAVE 10% OFF ICB PRODUCTS WITH DISCOUNT CODE: 02ICB10 Offer online only!
References:
1. The American College of Foot & Ankle Orthopedics & Medicine. Prescription Custom Foot Orthoses – Practice Guidelines, December, 2006
2. COLLINS N, BISSET L, MCPOIL T, VICENZINO B. Foot Orthoses in Lower Limb Overuse Conditions: A Systematic Review and Meta-analysis. Foot Ankle Int. 2007;28(3):396-412.
3. RICHTER, Randy R. PhD, PT; AUSTIN, Tricia M. , PhD, PT, ATC; REINKING Mark F. , PhD, PT, ATC, SCS. Foot Orthoses in Lower Limb Overuse Conditions: A Systematic Review and MetaAnaiysis— Critical Appraisal and Commentary