Achilles pain can apply to a number of conditions that impact upon the Achilles tendon area. Generally most surgeons refer to any condition that elicits pain in the area of the Achilles attachment as Achilles tendonitis. Specifically, the makeup of the word is, ‘tendon’ meaning tendon and – ‘itis’ – a suffix used in pathological terms that denote inflammation with its origin being from the Latin language.
Different professions have sort to be more specific in the description of the condition and thereby more closely define this area of pain to design better treatment regimes. Terms such as Achilles tendinopathy, tenopathy, tendinosis, partial rupture, paratenonitis, tenosynovitis, tendovaginitis, peritendinitis, and achillodynia have been used to describe the problems of non-insertional pain associated with this tendon1.
In this blog we will be considering the overuse and inflammatory condition that is associated with Achilles pain, with pronation and supination as main contributory elements.
The biomechanics of the condition starts at heel strike in the gait cycle. After heel strike the foot accelerates into an excessively pronated position and the calcaneus is everted, increased medial tendoachilles traction occurs and may result in transverse shearing of the tendon and sheath, eliciting inflammation and pain.

Additional stress is encountered at heel lift as inversion of the calcaneus is assisted by the gastrocnemius and soleus muscles.
Achilles (pain) Tendonitis is similar in its biomechanical action to Plantar Fasciitis in that as the foot pronates, it causes a tractional pull on the attachment and continued Subtalar Joint pronation for any length of time, will allow continuation of the tearing of the sheath. Inflammation and swelling will occur as this continues to takes place.
This action of continual stretching and bending is likened to constant bending of a piece of wire in which the wire heats up in the area of flexion and eventually dips/bends and snaps. The heat generated in the wire is similar to the inflammation that occurs in the Achilles in which inflammation is evidenced when constant stretching and strain occurs. If the patient excessively pronates constantly, the inflammation will be more prominent on the medial side and conversely, supination on the lateral side as the patient strikes with a high strike angle laterally and then proceeds to pronate through midstance, then to toe-off. Inflammation can occur on both sides due to this being the biomechanical pivot point.
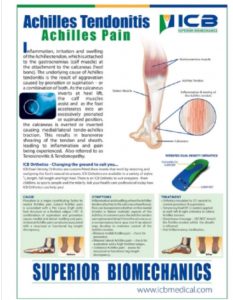
The engineering graph below gives an insight into stress studies that have been conducted on building material, however, this principle has been adopted by bio mechanists as they apply it to ‘body engineering’.
Looking at the graph we have stress and strain vs time or physiological range. A to B is any material that returns to its shape over a period of time – in this case the stress and strain on the Achilles tendon is associated with abnormal foot function.
B-C is the yield point – the point at which the Achilles tendon is stretched so much that it is unable to return to its original shape. When this transpires inflammation occurs and pain is felt. At this point the patient seeks medical help, and often the symptom is treated, however the biomechanical cause may go untreated. With rest the pain may subside, repetitive stretching of the Achilles tendon will move the condition towards point D, i.e. continual flare up of the Achilles tendon may take place.
Point D is where complete rupture of the tendon may occur or a posterior calcaneal compensatory spur may develop as the body seeks to maintain the attachment.
Changes to the patients’ lifestyle e.g. job change or a new exercise routine may cause additional stress being placed on the biomechanical structure, causing aches and pains to occur in the ankle, knees, hips or even lower back pain. The additional stress on the body will most likely present as pain in an existing area of weakness, and be associated with biomechanical anomalies causing periods of pain and discomfort to occur.
Treatment
The position or point of pain can be a clear indicator of underlying factors. When pain is on the medial side of the Achilles, it is often associated with Subtalar Joint pronation – as it causes the medial aspect of the Achilles tendon attachment to elongate and tear, and will need to be treated with an anti-pronation orthotic.
When the pain is on the lateral side it may be associated with a high forefoot valgus or a high supination angle that causes the lateral attachment to elongate and possibly tear and should be treated with a forefoot valgus addition. If the rearfoot (calcaneus) is flexible a lateral posting can be applied.
Pain in the centre or both sides of the Calcaneal attachment often this is associated with supination at heel strike with ground reaction forces on the lateral side encouraging the foot to move into a pronated position at midstance to toe-off phase of gait. The lateral to medial movement may cause this to be the pivot point of traction of the Achilles tendon and will inflame or flare up the medial and lateral side of the tendon sheath and bursa. Treatment will require both treating both excessive pronation and excessive supination by using orthotic additions attached to the orthotic device to support the arch and address any forefoot valgus deformity.
When prescribing orthotics always check for any structural leg length discrepancy, especially if unilateral Achilles pain is being experienced as the longer leg can, as compensation, excessively pronate to level the pelvis.
Repetitive stress and strain on the Achilles over a period of time may cause a posterior calcaneal spur to develop as compensation. Surgical intervention to remove a Posterior Calcaneal Spur can be accomplished without detachment of the Achilles tendon. Successful surgical intervention on a posterior calcaleal spur is more successful than surgery on an Inferior Calcaneal Spur (heel spur).
Additional Treatment Option
• Foot Mobilisations: especially to check if the calcaneus is displaced posteriorly, as this will exert additional traction pressure on the Achilles.
Short term use of a heel lift on both feet (in addition to an orthotic device) to shorten the gastrocnemius muscle and relieve pressure on the Achilles attachment. Do not allow the patient to continue wearing the heel lift for more than 2-3 to reduce Gastrocnemius shortening inflammation should subside in this period of time..
• Acupuncture (or dry needling): at the point of pain can be attempted to reduce to the swelling and inflammation.
• Non steroidal Anti-inflammatory Medication: only in the early stages of the condition.
• Cortisone: is initially effective, however it weakens the ligament structure and it is advised to limit use to one or two occasions. A more conservative approach will be far more beneficial to the patient.
Corticosteroid injections into the region of pain is a common treatment for plantar fasciitis and often Achilles pain. However, such injections have been associated with serious side effects2. Acevedo and Beskin3 reported that in a group of 765 patients with a clinical diagnosis of Plantar Fasciitis, 51 were diagnosed as having a plantar fascia rupture. Of these 51 ruptures, 44 (86%) were associated with corticosteroid injection4. Therefore reliance upon this form of treatment is discouraged for Achilles pain also and a more conservative approach adopted.
Get a FREE Achilles Tendonitis Poster
References
1 Khan KM, Maffulli N. Tendinopathy: An Achilles’ Heel for Athletes and Clinicians. Clin J Sport Med.1998 Jul;8(3):151-42.
2. LEMONT Harvey, DPM. Plantar Fasciitis A Degenerative Process (Fasciosis) Without Inflammation
3.AMMIRATI Krista M. BS, USEN Nsima, MPH May/June 2003, Vol 93, No 3 Journal of the American Podiatric Medical Association
4. ACEVEDO JI, BESKIN JL. Complications of Plantar Fascia Rupture Associated with Corticosteroid Injection. Foot Ankle Int. 1998 Feb;19(2):91-7.
General REFERENCES: BRUNKER, P., & KHAN, K. (1993) Clinical Sports Medicine, Sydney: McGraw-Hill Book Company