Leg length Inequality and the pathogenesis or the origin and development of the condition, is and will always be, a controversial subject. There is a wide variance of opinion on the significance of structural leg length and the various methods for measurement.
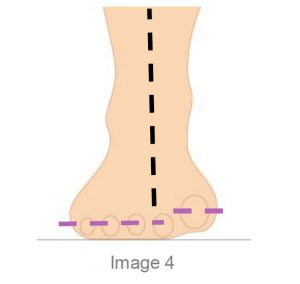
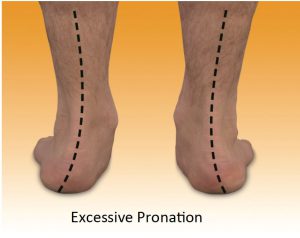
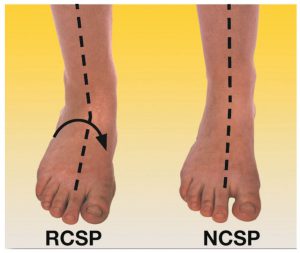
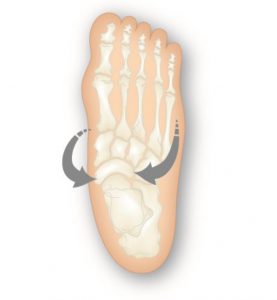
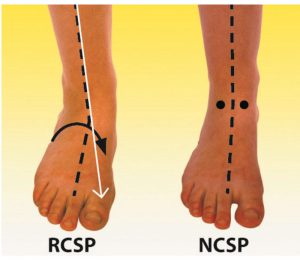
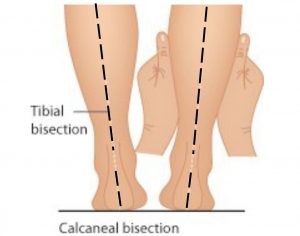
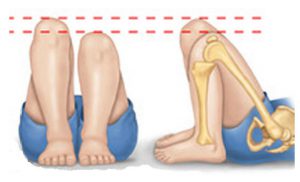
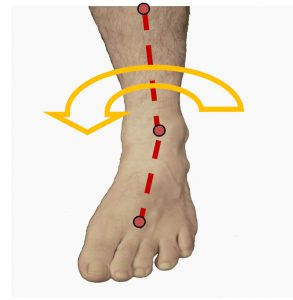
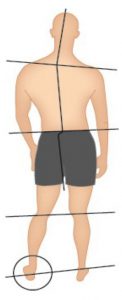
Measuring of structural leg length when treating with orthotic therapy is necessary as undiagnosed structural leg length compensation will be affected when orthotics are prescribed for the patient. The natural body compensations for leg length difference can range from long leg flexion, to short leg supination amongst others as the body seeks to rebalance pelvic alignment. The most common compensation is long leg excessive pronation, accounting for around 80% of the long leg compensations. However in very large structural differences, short leg toe walking and short leg excessive pelvic drop may be taken up as compensations with inevitable upper spine outcomes such as functional scoliosis.
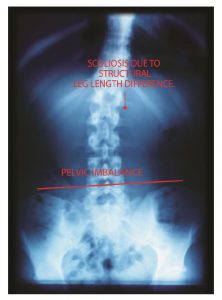
Managing a treatment protocol to assist in minimising issues can be difficult especially if the spine is fixed, that is, the spine (or spinal segment) is not mobile or correctable by conservative means. This is often referred to as a Fixed Sagittal Imbalance (FSI) and conservative treatment looks to make the patient as comfortable as possible when surgical intervention is not undertaken.
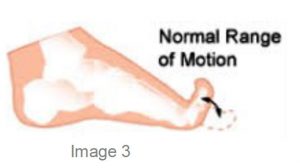
In this newsletter we will focus on conservative treatment methods that can be adopted when the osseous structure is mobile.
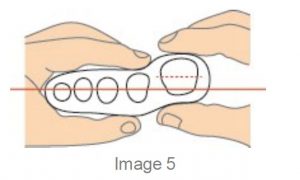
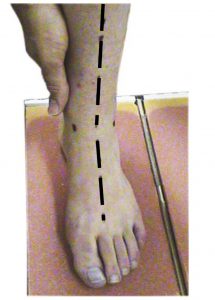
Assessment for structural leg length difference as part of the initial assessment will avoid removal of undiagnosed compensations and provide an understanding of the size and extent of the leg length difference .
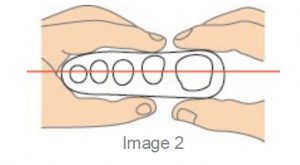
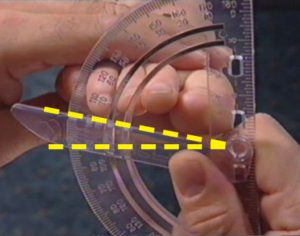
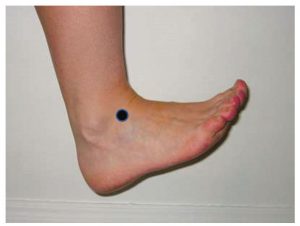
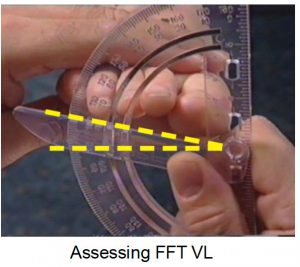
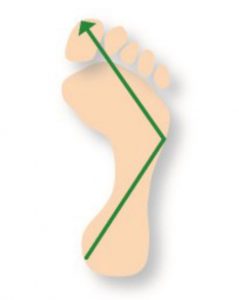
There are many ways to measure leg length, tape measure, x-ray, physical assessment of the limbs such as Palpation for Supine Medial Malleoli Asymmetry Technique 1
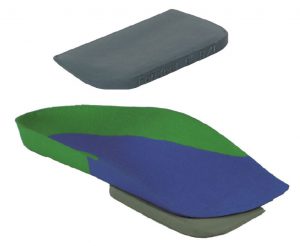
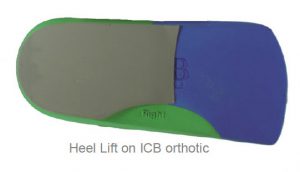
ICB provides both 10mm and 15mm extended heel lifts which can be used when the patient has custom made orthopaedic shoes or is wearing boots or the shoe has extra depth in the heel cup as they can be accommodated inside the shoe wear.
The extended heel lift is designed with a longer profile to support the mid foot and eliminate any mid foot collapse which can occur in Heel lift Larger than 8mm high. ICB regular heel lifts are available in S/M/L heel 4/6/8mm and the extended model is available in 10 &15mm.
Generally leather dress shoes can cope with a heel lift up to 6- 8mm (depending upon heel cup height) when added to the orthotic, higher than that the patient may complain that their heel is slipping out of the shoe.
Therefore, alternate shoe styles or modifications need to be considered to accommodate for large structural differences. When recommending shoes with orthotics a deep heel cup is an advantage.
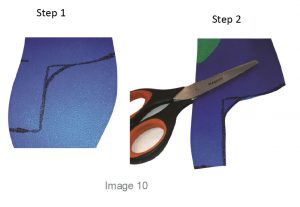
Cross trainers and boots are able to accommodate a larger amount of heel lift in the heel cup, however this may limit the patient to a smaller selection of fashion shoe styles. A solution may be to add maximum amount to the orthotic and then modify the patient’s shoe to achieve the best result. (see below)

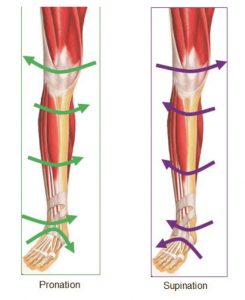
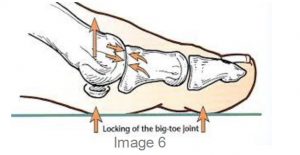
To incorporate an intrinsic lift, the sole of the shoe should not contain gel, air cushion pockets and have a base that is flat with no arch cut out. A boot maker can cut the EVA sole with a band saw, finishing behind the breakpoint or 1st MTPJ when the heel lift is less than 30mm. This will enable a normal walking pattern and toe off to occur.

Once the intrinsic heel lift in the shoe sole is over 30mm the cut in the sole must extend to the sulcus behind the phalanges and if a greater amount, to the end of the foot in a thicker ‘ramp’ like adjustment.
The patient featured presented with a condition that could be treated with orthotics , an additional heel lift or raise was recommended to be placed into the heel of the shoe by a boot maker or shoe repairer.
A temporary Heel Lift was used to validate the treatment suggestion note the RIGHT shoe with temporary extrinsic addition which successfully corrected the functional

Extrinsic Heel Lift under shoe heel (above)
scoliosis, this is the amount that should be added into the shoe sole.
Refer :The Orthotic Solution book p45
Note: It is recommended that both left and right feet are fitted with an orthotic, in addition to any heel lift requirements, to ensure the foundation of the body is balanced.
Generally most footwear will accommodate an orthotic with a 6-8mm heel lift addition (depending upon heel cup height). If a larger heel lift is required(10mm +), extra depth footwear or boots may be required – or alternatively, adjustments to the footwear to incorporate a partial lift into the sole of the footwear can assist.
Reference: 1. Gary Fryer 2005 : Factors affecting the intra-examiner and inter-examiner reliability of palpation for supine medial malleoli asymmetry .