Orthopedic terminology describes inversion as a frontal plane movement of the foot, where the plantar surface is tilted to face the midline of the body or the medial sagittal plane, the axis of motion lies on the sagittal and transverse planes, a fixed inverted position is referred to as a varus deformity1.
Inversion sprains are probably the most common foot sprain condition and they are often associated with pes cavus feet or a high forefoot valgus in relation to foot mechanics. The treatment of this type of condition will involve a combination of different modalities including orthotic therapy to stabilize the foot mechanics. Watch the video below for a short introduction.
The most commonly injured site on the foot is the lateral ankle complex, which is composed of the anterior talofibular, calcaneofibular and posterior talofibular ligaments.2,3,4,5
This article will focus on lateral sprain and pain associated with a pes cavus foot structure and a forefoot valgus deformity.

Repetitive lateral ankle sprain or lateral knee pain (or even lateral shin splints) is often diagnosed as ‘idiopathic’, closer examination of the biomechanical relevance needs to be pursued. The term ‘idiopathic’ is often used in this area as there seems no reason for the pain occurrence. The meaning of idiopathic is a derivative of the Greek word idios “one’s own” and pathos “suffering”, or ‘arising spontaneously or from an obscure or unknown cause’ 6
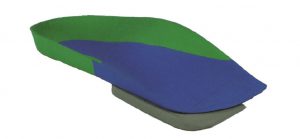
Pes cavus foot (high arch) structures (see Figure 1) appear to have a predisposition to lateral ankle sprains and present as a rigid structure and a supinated foot structure.
Patients with this foot structure will often complain that their joints are painful and when they walk without shoes on hard floors.
This type of structure will usually exhibit a forefoot valgus deformity meaning that:
‘The plantar plane of the forefoot remains everted relative to the plantar plane of the rearfoot when the subtalar joint is in neutral.’
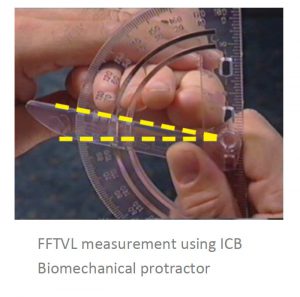
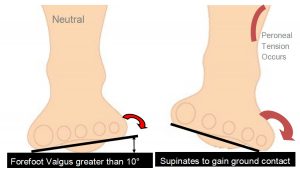
This deformity will have an impact on the patient in heel strike, midstance and toe off phase of gait. The patient who exhibits a pes cavus foot structure will often present with a (FFVL) Forefoot valgus greater than 10º and will often exhibit a plantar flexed 1st metatarsal (Boyd & Bogdan, 1993), encouraging the foot to strike laterally and eliciting pressure on the lateral aspect of the hip joint.
If the Forefoot valgus deformity is greater than 10º, the foot will often continue to supinate through the cycle, having a jar-ring effect on the upper structure, putting additional strain on the Lateral aspect.
When the foot is supinated it will stress on the peroneals and may cause elongation of the muscles and tendons, thus weakening the retinaculum and lengthening the peroneals and may cause the tendon to sublux off the lateral aspect of the malleolar.
The FFT Valgus deformity (in gait) encourages the foot to invert the foot, propulsion is delayed causing lateral instability and results in tension and tearing of the peroneal muscles, causing inflammation and tenderness, and difficulty walking. Lateral ankle sprains are more common than medial due to the fact that ligaments are weaker on the lateral side7.
Hence the lack of lateral stability can be caused by uncompensated or partially compensated rearfoot, a flexible forefoot valgus or osseous forefoot valgus (Boyd & Bogdan, 1993; Hollis et al, 1995; Shapiro et al 1994).
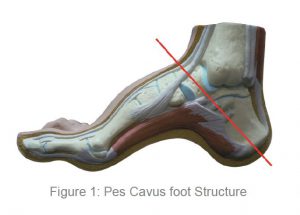
There are also certain biomechanical foot deformities that make some patients more susceptible to inversion sprains, such as, neurological deficits and supinated foot types which exhibit or function with a supinated calcaneus (Valmassy, 1996),
• In gait the FFTVL allows inversion of the foot to gain ground contact.
In summary, if a patient presents with lateral hip pain, knee pain, ankle strain or repetitive lateral inversion sprain, check for a forefoot valgus deformity and employ the following treatment suggestions to assist in alleviating the pain symptoms, whilst treating the underlying causation.
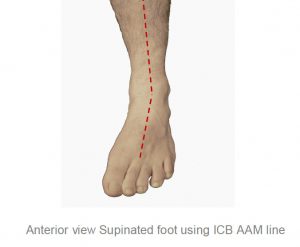
If the patient requires a forefoot valgus posting to be added to their orthotic devices remember that the measured forefoot valgus deformity commence by taking ½ the measured amount and gradually increasing until treatment is effected or the patients shoe wear is not able to accommodate.
If the forefoot valgus is very large say greater than 15º, a reduction in the posting size may be required to assist the patient in being able to accommodate the orthotic in the shoe box area.
Suggested Treatment Options for Lateral Pain:
• Deep tissue massage along the peroneal muscles or suction cups to break down scaring and adhesion.
• Orthotic device with an appropriately sized forefoot valgus addition applied (see Figure 4). Always start with a conservative sized valgus addition, and build up from there to assist compliance.
• Acupuncture at the point of pain.
• Lateral Prolotherapy to strengthen the lateral ankle ligaments to encourage proliferation of the lateral ligaments (formation of collagen fibres).
• Mobilisation of the cuboid joint, as this may become subluxed.
• For lateral ankle sprains use stabilising ankle strapping, in combination with the orthotic device.
The USA National Athletic Trainers’ Association (NATA) new guidelines for treating and preventing ankle sprains in athletes are as follows:
• Early use of non-steroidal anti-inflammatory drugs (NSAIDS) post injury
• Functional rehabilitation rather than immobilisation for grade I and II ankle sprains
• Prophylactic ankle supports for athletes with a history of previous ankle sprains
• Immobilisation with a rigid stirrup brace or below-knee cast is recommended for grade III sprains for at least 10 day followed by controlled therapeutic exercise.

REFERENCES :