Hallux limitus / rigidus is defined as a degenerative arthrosis of the first metatarsophalangeal joint characterised by a decrease in first metatar-sophalangeal joint range of motion and eventual absence of motion.1
* The Morton’s extension is a 3°- 4˚ ramp under the phalange to allow the patient to propel off at toe off stage of gait. To create a Morton’s extension you can use an ICB 4° Forefoot wedge. and trim.
The progressive nature of the condition was first documented by Cotterill2 and Davies-Colley3 in literature over a century ago, in which they described hallux limitus / rigidus as a progressive condition producing a severely painful and rigid big-toe joint.
Hallux Limitus is assessed as being evident when movement of the great toe (hallux) is restricted to less than the normal range of motion or flexion to 65 – 75 degrees.
Flexion in the big toe assists to maintain the correct walking gait action to perform normal functions such as stooping down, climbing up, or even standing. For these reasons this disorder can be very troubling and even disabling.
Early signs and symptoms include:
• Pain and stiffness in the big toe
• Abduction of the foot in gait to reduce stress on the 1st MTPJ at toe off.
• Swelling and inflammation around the 1st MTPJ
The main contributing factor biomechanically is as follows:
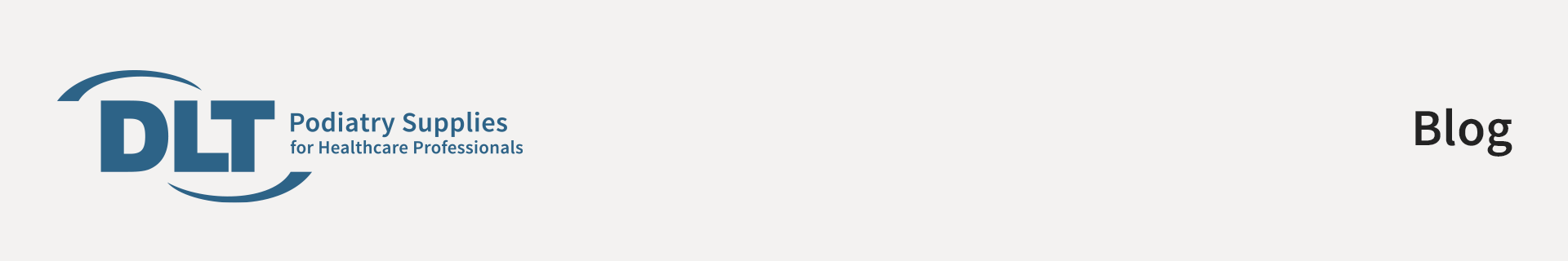
1. A long 1st metatarsal shaft
2. A short 1st metatarsal shaft In the case of the long metatarsal shaft the 1st MTPJ strikes the ground early and dorsiflexes the 1st metatarsal head. As this happens it restricts the proximal phalange from propelling over the 1st MTPJ and creates an impingement of the joint. Osteoarthritic changes result in the metatarsal joint and narrowing of the joint space leading to hallux limitus or a joint with limited movement. If action is not engaged to prevent it will eventually lead to hallux rigidus or joint ceasure.
A short metatarsal shaft will adduct to the midline of the body to gain ground contact, as this happens the metatarsals will plantarflex and rotate, and the ground reaction forces will cause dorsiflexion of the 1st metatarsal head.
This, when combined with the pronation factor, will create impingement at the tarso metatarso joint and reduce the proximal hallux’s ability to propel over the joint.

The tarso-metatarsal joint will in this instance be stressed and the ability of the proximal hallux in the propulsive phase of gait to flex to its normal range of motion will be reduced as it impinges or jams the 1st MTPJ.
Often this is referred to as a Functional Hallux Limitus (FHL) as it combines with the pronation factor and ground reaction forces to limit movement. Limited flexion will usually cause 3 types of outcomes:
1.An adductory twist: this is where the calcaneus pivots medially at the propulsive phase of the gait cycle. This is in turn assisted by the external hip rotators such as piriformis, gluteals and ITB’s, and as this takes place medial ground reaction forces (GRF) put pressure on the 1st MTPJ. As the patient attempts to toe off this causes the hallux to deviate and develop me-dial callosity.
2.The distal phalanx of the hallux be-comes the alternative propulsive mechanism which is due to limited joint mobility at the 1st MTPJ, thus causing dorsiflection of the distal hallux with secondary action of nail trauma & nail thickening ( onychogryphosis). The result of this is that many patients wear through the dorsal aspect of their shoe or socks.
3. Abduction of the foot in gait to reduce the impact upon the 1st MTPJ resulting in increased medial pronatory forces.
Correctly aligned and modified orthotic device will alleviate these outcomes and allow the 1st MTPJ to function within the parameters of the structural abnormalities of the foot of the presenting patient.
Once the foot structure is realigned and maintained in the ideal / neutral position pressure is taken off the 1st MTPJ and increased flexion in the joint can be achieved.
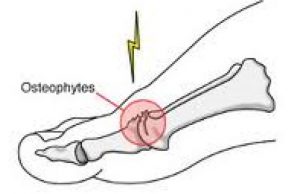
Rx : Treatment for a long 1st metatarsal shaft- an orthotic to lift the proximal hallux and at the same time deflect the 1st MTPJ by way of a depression placed under the joint using a heat gun on a 100% EVA orthotic device – using a full length orthotic style is best (see fig. 1 below). Composite orthotic products have limited heat-ing ability and do not allow for easy deflection creation.
Rx: Treatment for a short 1st metatarsal shaft is more complicated as we need to attack the problem on a num-ber of fronts:
1. Correct the pronation factor using an orthotic device moulded to the patient’s ideal / NCSP (Neutral Calacaneal Stance Position) which will control rearfoot eversion (pronation). Generally a device with between 4˚-6˚ rearfoot varus will give the required control.
2. The orthotics should control and correct both the Subtalar and mid tarsal joint pronation together using a device that can be moulded to effectively follow the con-tour of the patients arch to reduce longitudinal arch col-lapse (which would encourage the foot to evert during the propulsive phase) whilst maintaining rearfoot con-trol.
3. Use a ‘Morton’s extension addition’* to lift and sup-port the hallux and allow the hallux to propel over the joint (see Fig. 2). The Morton’s extension lifts the 1st MTPJ to level with the lesser metatarsal joints and allow the proximal phalange to maintain its position and stops the 1st MTPJ from plantarflexing & rotating which encourages the pronation effect.
Ultrasound or other physical therapy modalities may be undertaken to provide temporary relief.
Non-steroidal anti-inflammatory drugs (NSAIDs), may be pre-scribed to help reduce pain and inflammation in the 1st MTPJ.
Supplements such as glucosamine-chondroitin sulfate and some vitamins and mineral supplements may also be helpful .
Differential Diagnosis:
Check for gout, rheumatoid and Psoriatic arthritis.