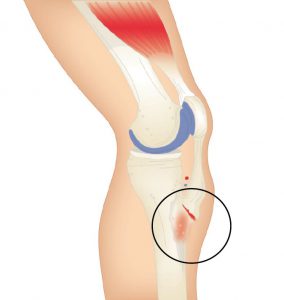
Osgood–Schlatter disease or syndrome, also known as Apophysitis of the Tibial Tubercle, is an irritation of the patellar ligament at the tibial tuberosity occurring at the tendon-bone junction of the patellar tendon and the tibial tuberosity.1
The condition is named after Robert Bayley Osgood (1873-1956), an American Orthopedic surgeon and Carl B. Schlatter, (1864-1934), a Swiss surgeon who described the condition independently in 1903.
Watch the video below about Osgood–Schlatter disease below.
General medical opinion is that Osgood Schlatter Disease, is caused by repetitive stress or tension on the growth plate of the upper tibia (the apophysis), which can be complicated by growth spurts and biomechanical deformities or anomalies. In general medical circles it is often called ‘growing pains’ and is similar in bio-mechanical dysfunction to Severs Condition, however occurring in this instant at the tibial tuberosity being characterised by inflammation of the patella tendon and surrounding soft tissues at the point where the tendon attaches to the tibia.
This condition appears to afflict children who are growing fast and often have external Tibial Torsion condition combined with Internal Tibial Rotation associated with excessive pronation.
Osgood-Schlatter’s Disease, is we believe, caused by repetitive stress or tension on the growth plate of the upper tibia (the apophysis), which can be complicated by growth spurt syndrome and biomechanical deformities or anomalies. The cause is similar in biomechanical operation to Sever’s Disease, except that it occurs at the tibial tuberosity and characterised by inflammation of the patella tendon and surrounding soft tissues at the point where the tendon attaches to the tibia.
As stated, it is usually young people who suffer with this disease – experiencing pain just below the knee joint and patella which usually worsens with activity. It is also associated with an avulsion injury (stretching the tendon so much that it tears away from the tibia and in extreme cases takes a fragment of bone with it – See Figure 2).

A bony bump may appear on the up-per edge of the tibia (below the knee cap) that may be particularly painful when external pressure is applied. It has been misdiagnosed in the past in Australia as “surfer’s knee” (a myth that only surfboard riders suffered from the condition). The hinge motion of the knee is not actually affected.
Most commonly Osgood Schlatters Disease affects active young people, particularly boys between the ages of 10 and 16 who play games or sports that include frequent running and jumping.
In a retrospective study of adolescent athletes actively participating in sports showed a frequency of 21% reporting the syndrome compared with only 4.5% of age-matched non-athletic controls2. Bilateral symptoms are observed in 20–30% of patients indicating that there is a higher incident of unilateral occurrence lead-ing one to deduce that in the unilateral cases, structural leg length or other unilateral biomechanical anomalies may be a contributing factor.
Symptoms of Osgood Schlatters Disease include:
• Pain over the tibial tubercle
• Swelling over the tibial tubercle
• Weakness in the quad muscle group
• Increased pain & swelling with activity
• A visible lump at the base of the knee cap
• Pain to the touch over the affected area.
Often the pain may last only a few months or may recur until the child stops growing.
Not a lot has been written about the effect of the combination of a growth spurt combined with both pronation or supination, and internal and external tibial torsion. However, children appear to experience more pain and resultant damage to the attachment when these factors occur in combination.
The pain (and resultant effects) become more noticeable during activities that require running, jumping or going up or down stairs and is most common in young athletes who play football, soccer, basketball, netball or who are involved in gymnastics and ballet.
Contributing Factors whilst the Child is still growing
1. Excessive Pronation:
As the foot pronates internal tibial rotation occurs. The body’s mechanism of compensation causes the ITB’s and abductor muscles to tighten in the opposite direction causing the patella to laterally and superiorly displace, hence causing a tractional pull on the tibial tuberosity.
2. Supination & Pronation:
Because of the anterior position of the tibial tuberosity, when the foot supinates due to a FFT valgus deformity less than 10 degrees in the swing phase of gait, the foot lands laterally then the ground reaction forces (on the lateral side) propel the foot into pronation with the same effect above.
3. Internal Tibial Torsion:
Internal tibial torsion will cause the foot to rotate the tibial condyle medially. The ITB’s and gluteals then tighten and come into action as an external rotator of the femur as the compensatory mechanism causing external rotation above the knee and internal rotation below the knee.
The two rotation actions have an effect on the patella and its tendon attachment also causing the tibial tuberosity to stretch and pull.
4. External Tibial Torsion: This causes the foot to externally rotate in the swing phase of gait, the iliopsoas and adductor muscle groups combined to provide compensation at the late swing phase, causing the foot to straighten and land laterally (same effect as 2). Then the ground reaction forces cause the foot to pronate with the help of the psoas pull resulting again in internal rotation above the knee and external tibial torsion position increases tractional forces on the patella and its attachment.
Treatment
• Orthotics moulded to the patient’s Ideal/Neutral Calcaneal Stance Position to realign and hence reduce the effect of tibial rotation.
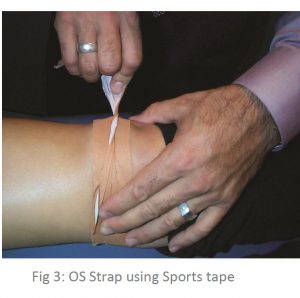
• Combine orthotic therapy with strapping: use an Osgood Schlatters strap (see below) to reduce the tension on the attachment at the growth plate whilst the child is playing sport (see Figure 3).
Stretching may exacerbate the tearing – alternatively use deep friction massage to help in pain relief.
• R.I.C.E
Active children may experience shortening of the muscles whilst growing, which coupled with biomechanical anomalies = predisposition to Osgood Schlatter.
Contraindications
It is important to differentiate from malignancy, infection, fracture, tendonitis and Sindling-Larsen-Johansson Disease. Initially the diagnosis is based on clinical signs and symptoms including: pain, heat, tenderness and local swelling with prominence at the tibial tuberosity. X-ray is required to establish the extent of the condition.
Steroid injections are discouraged as this may cause weakening of the infra-patellar ligament, scaring and fat necrosis.