Knee pain is a common condition experienced by people of all ages, and levels of activity. Knee pain is a problem that can be experienced due to many contributing factors, Including: increased Q-angle, genu-valgum and genuvarum, muscle tightening through the gastrocnemius, iliotibial band and VMOs, hyper-extension of the knee and tibial rotation and torsion, bakers cyst, connective tissue disorders such as lupus .
When discussing knee pain, terms such as ‘Retro Patella pain’, ‘Patella Femoral Dysfunction’, ‘Medial Compartment Syndrome’ or ‘Ilio Tibial Band Friction Syndrome’, come to mind. However, from ICB’s experience, these conditions are simply descriptions of knee pain. Knee can be affected by trauma, foot mechanics or issues at the hip. Trauma issues are not discussed in this article , rather we focus on the other two areas, both of which can affect the operation of the knee.
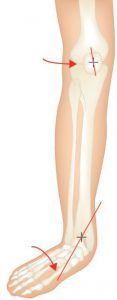
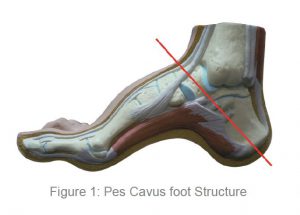
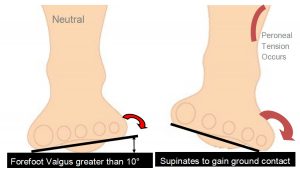
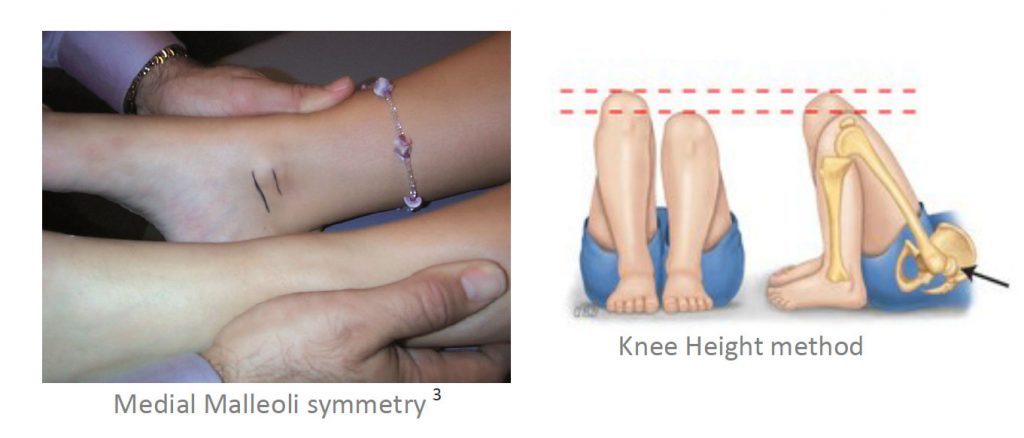
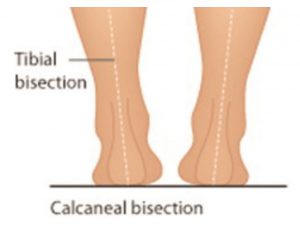
If the patient’s pain is idiopathic (i.e.. no known cause or trauma), excessive pronation and excessive supination may constitute the underlying cause of the problem – as outlined by Michaud, 1997 1. Michaud states that for every 1˚ of pronation the tibia internally rotates 1˚, which in turn impacts on the knee joint, as it takes the stress that is generated by the tibial rotation.
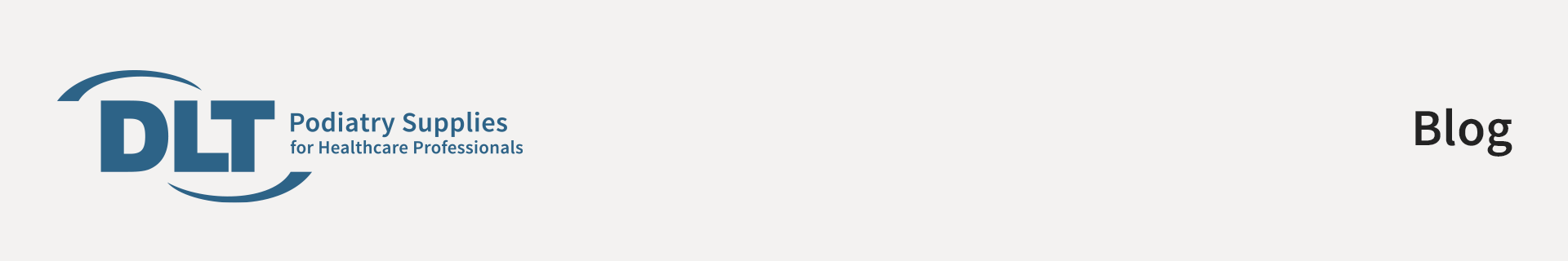
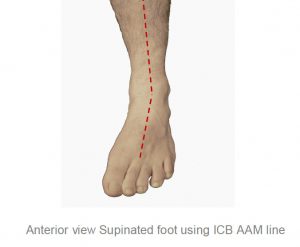
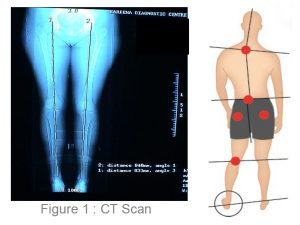
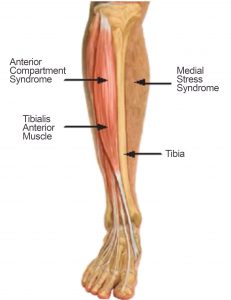
Tibial rotation describes the rotation of the tibial shaft and is different to tibial torsion. Tibial Torsion is a twisting in the osseous structure of the tibial shaft. Internal Tibial rotation is associated with excessive pronation, medially displacing the patello femoral path and encouraging lateral displacement of the patella. Internal Tibial Rotation is a common problem and elicits pain under and around the medial aspect of the patella – especially with excess loading activities such as running and jumping.
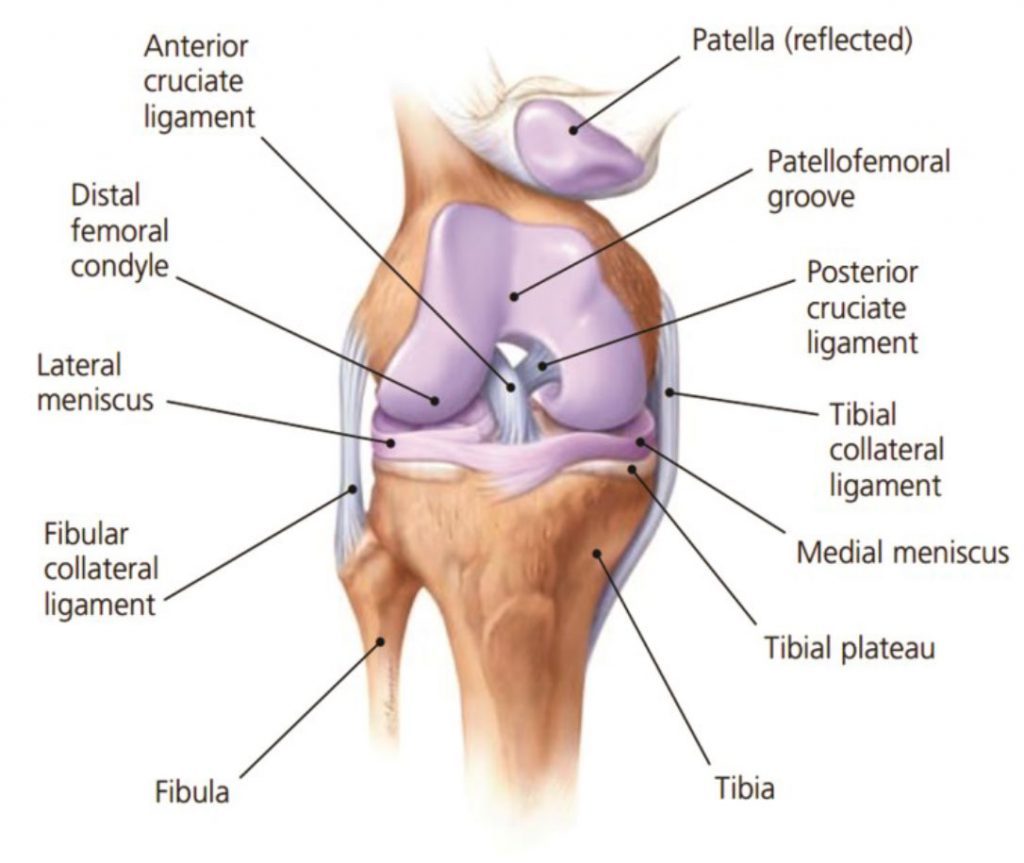
Internal tibial rotation is able to con-tribute to medial collateral strain on the ligament structures that wrap around the medial aspect of the knee and lower leg (Cosgarea, 2002)
To treat pain associated with internal tibial rotation, give VMO strengthening exercises , knee strapping, and other strengthening exercises – all of these are valuable treatment options, however, these methods, no matter how beneficial, only treat the symptoms. Controlling and stabilising the foundation is a key to successful treatment of medial knee pain.
CAUSES OF MEDIAL KNEE PAIN
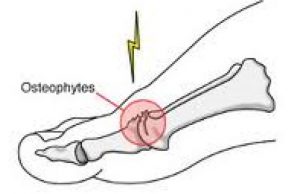
A major cause of medial knee pain is excessive pronation which causes the medial collateral ligament to elongate resulting in the weakening of the VMOs and the ITBs tightening. A con-sequence of this action is external rotation of the femur as compensation. As the ITB and piriformis muscles compensate to reduce medial rotation, the patella begins to track on the lateral aspect of the femoral condyle and a grinding and crackling is felt on the flexion to extension.
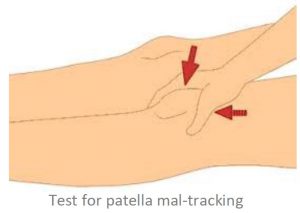
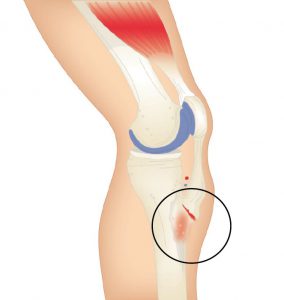
Strapping, using the McConnell technique and strengthening VMOs is a good treatment method, however it will not correct the problem – strapping will only assist in pain relief, and the condition will constantly re-occur until the knee has degenerated or become Osteo-Arthritic, and may eventually require surgical intervention.
A basic requirement to reduce rotational stress on the knee is STJ and MTJ control and correction.
BIOMECHANICAL TREATMENT
• McConnell strapping technique to control lateral/medial patella displacement, in conjunction with low dye strap-ping to mimic the support and control of an orthotic de-vice. Low dye strapping, however, is only a temporary treatment.

Low Dye taping to imitate wearing orthotics.
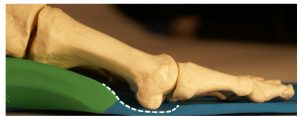
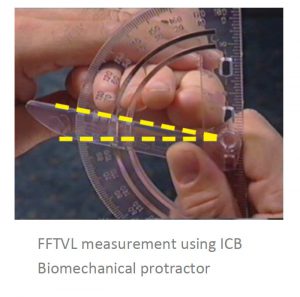
• ICB Orthotics moulded to the patient’s Ideal/NCSP (Neutral Calcaneal Stance Position) to control abnormal STJ and MTJ pronation, by aligning the calcaneus with the lower 1/3 of the tibia and limiting the joint to its original function as a hinge joint.
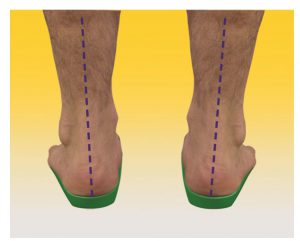
Rearfoot correction using ICB Orthotic with intrinsic 5° Rearfoot varus.
• Strengthening VMO exercises whilst correcting the feet with orthotics, and stretching the ITBs.
• Mobilisation of the knee joint may also be useful.
• Acupuncture can be performed at the point of pain to aid pain relief.
• Runners may require increased rearfoot varus wedgeing to compensate for the higher tibial varum angle at heel strike, during the running cycle.